DAILY NEWS… One of the main reasons South Australians threw out their single-term Mitchell State Government last Saturday was ambulance ramping, which begs the question of why NSW residents are prepared to put up with ramping, slow ambulance response times, long emergency department waits and dangerous elective surgery delays. Jackie Pearson looks at the latest Bureau of Health Information (BHI) Healthcare Quarterly results for the period of October- December 2021 and asks how bad it will need to get before NSW voters start baying for ballot box blood.
The most striking anti-Liberal-Mitchell Government posters hanging off telegraph poles in Adelaide last week depicted the face of the state’s (now former) Premier Steven Marshall on a cigarette packet familiarly branded ‘M’ (for those who have been around long enough to remember branded cigarette packets).
The implication was that the Marshall Government’s health policies were as dangerous as tobacco. In particular, “ramping”, the issue of patients taken to a hospital emergency department via ambulance having to wait on the ambulance trolly and in the care of an ambulance officer for an extended period of time, before being transferred to an emergency bed and seen to by hospital staff.
Ramping has been an accepted fact of life in NSW for decades but South Australian voters were not having a bar of it.
Post-election the victorious new Labor Premier Peter Malinauskas declared the Liberals’ poor performance on health, and particularly the escalation of ramping, as one of the main reasons why voters threw the Marshall Government out after one term.
Why then are NSW voters prepared to accept a broken health system, corruption, pork barreling and a litany of other sins from its political class with a shrug of the shoulders? We will find out in March 2023 when the next NSW election is held.
Meanwhile it is clear from the latest Bureau of Health Information (BHI) data that if South Australian voters had to put up with the NSW health system there would be insurrection.
The BHI data for the October to December 2021 quarter also indicates that the socio-economic profile of the Local Health District has a bearing on how long you will have to wait for an ambulance, emergency department care or elective surgery. It appears that people living in poorer areas of NSW get poorer care.
Let’s take the latest statistics for the Central Coast Local Health District as an example of how this plays out. The two major hospitals, Gosford and Wyong, service a percentage of aged pensioners that is above the state average, a percentage of people living with disability which is above the state average, a disproportionately high level of cancer clusters, a disproportionately low level of people who have completed tertiary education and, hence, a rather high number of lower-than-average income earners. As the number of bulk-billing GPs within the Central Coast Local Health District falls, dependence on the two emergency departments rises. Going to emergency or calling an ambulance is the only way some residents can have their health needs seen to.
State Member for Gosford, Liesl Tesch, has highlighted that for Gosford Hospital ambulance and emergency department wait times increased substantially when compared to the same quarter in the previous year: only 43.8% of Priority 1 calls to ambulances were responded to within 15 minutes, (down 10.2%); only 53.9% of treatment was started on time (down 7.3%); the number of patients on the waiting list for elective surgery at Gosford Hospital increased by 17% to 3,253.
And was ramping a problem at Gosford Hospital? Yes, there was a 6.9% decrease of patients transferred by paramedics to Emergency Department staff within 30 minutes.
Tesch said she was deeply concerned by these results following the Perrottet Government’s decision to close Ettalong Ambulance Station. A new station is to be built in the grounds of the Woy Woy Hospital (which doesn’t have an emergency department despite supporting a population of around 40,000).
“This is dangerous for everyone in our healthcare system – not only for the patients but also for the staff who are pushed to extreme levels as they try to serve the needs of our community,” she said.
“Premier Perrottet cannot even blame COVID for these results, it has been brewing for years because of the Liberal Government’s lack of investment in our essential services.
“After two absolutely grueling years dealing with the COVID-19 pandemic, our doctors and nurses deserve appropriate patient-to-healthcare professional ratios, and so does our community.
“While an increase in nurses and doctors is desperately needed here I know that this doesn’t mean a better ratio and while additional staff are hired, simultaneously the Government is taking away our Ettalong Ambulance Station, where the staff are not guaranteed a position at the new location.
“It is blatantly clear more needs to be done to fix our struggling health services and staff on the Central Coast. I demand that the Perrottet Government commit to resolving this crisis and closing down key parts of our local healthcare system is not the way to do it.”
Tesch is, of course, concerned with her own electorate, but a comparison of the Central Coast Local Health District with Sydney, the mid-North Coast of NSW and the whole state over five and 10 years reveals that the whole LHD is struggling across a range of measures.
For instance, locals on the Central Coast know that you need to take money, your phone charger and a good book with you if you need to visit either the Wyong or Gosford hospital emergency department because you’ve got a roughly 50:50 chance of being there for more than four hours. The October to December 2021 numbers were the worst for time spent in a Central Coast ED since 2012 – that’s a year after the last time NSW voters threw out a state government. And the Central Coast LHD’s performance on this measure is substantially worse than Sydney, Mid-North Coast or the whole state.
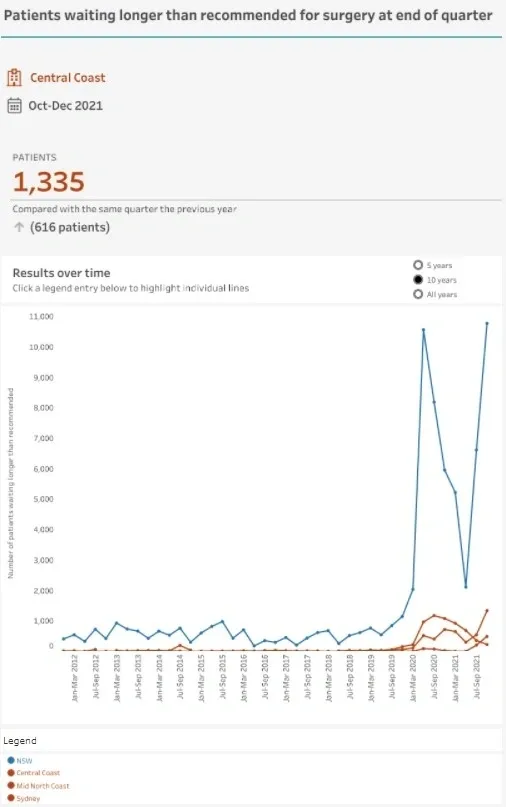
The next measure we looked at was the number of people waiting more than the recommended time for elective surgery. It shows that from one quarter to the next the number of patients waiting more than the recommended time for their elective surgery almost doubled.
That would be an easy metric to blame on the COVID pandemic and onset of Omicron during the October to December quarter. However, the same spike did not occur in the LHDs of the Mid North Coast or Sydney and the Central Coast’s spike was substantially more noticeable than that stat for the whole of NSW.
The third metric we considered was ambulance responses within 10 minutes to life threatening cases. We weren’t given the option of comparing the Central Coast LHD with other LHDs for this measure but again the performance worsened. Around 61% of life threatening responses occurred within 10 minutes a decrease of 5.7% on the previous quarter and a low-point for the LHD since 2016.
What can you do?
These statistics, and the comparison between what SA voters will reject and what NSW voters will accept calls to mind that old saying that “you get the government you deserve”.
The worst thing anyone can do is blame these trends on the ambulance officers, paramedics, nurses and doctors who work in the public system. They are doing their very best under extraordinary and “unprecedented” circumstances.
This is a systemic problem that has been created over decades by a succession of NSW Governments who have failed to adequately fund the public health system. Sadly poorer communities who are more likely to be dependent on ambulance and hospital care, appear to be copping the brunt of those successive poor funding models.
Surely the numbers quoted in this article are simply not good enough. To find out how your nearest hospital or your Local Health District performed you can go to the Bureau of Health Information’s Healthcare Quarterly results https://www.bhi.nsw.gov.au/data-portal and see for yourself.
We are very fortunate to live in a state and a country where such information is available to the public. Making it available is great but if the general public does not demand higher standards of care, better funding, nurse-to-patient ratios, more bulk billing general practices, more focus on preventative health measures, the system will keep getting worse.
The BHI portal is easy to use so exercise your democratic right to get informed about your local hospital and local health district. If it doesn’t stack up against others, give your local member a call, write to the NSW Health Minister and Shadow Health Minister and tell the Premier what you think.
And when your turn at the ballot box comes next March think carefully about the policies you are prepared to live with and act accordingly.


